Parasites:
Parasitism is a non-mutual symbiotic relationship between species, where one species, the parasite, benefits at the expense of the other, the host. Traditionally parasite referred primarily to organisms visible to the naked eye, or macroparasites.Parasite now includes microparasites, which are typically smaller, such as protozoans, viruses and bacteria.Unlike predators, parasites do not kill their host, are generally much smaller than their host, and will often live in or on their host for an extended period. Both are special cases of consumer-resource interactions. Parasites show a high degree of specialization, and reproduce at a faster rate than their hosts. Classic examples of parasitism include interactions between vertebrate hosts and tapeworms, flukes, the Plasmodium species, and fleas. Parasitism differs from the parasitoid relationship because parasitoids generally kill their hosts.(A parasitoid is an organism that spends a significant portion of its life history attached to or within a single host organism in a relationship that is in essence parasitic; unlike a true parasite, however, it ultimately sterilises or kills, and sometimes consumes, the host. Thus parasitoids are similar to typical parasites except in the more dire prognosis for the host)
Types:
Parasites are classified based on their interactions with their hosts and on their life cycles. An obligate parasite is totally dependent on the host to complete its life cycle, while a facultative parasite is not
Ectoparasites:
[Human head lice (Pediculus humanus capitis)]
Parasites that live on the surface of the host.
Endoparasites:
(Schistosoma mansoni is an endoparasite that lives in human blood vessels.)
Those that live inside the host (including all parasitic worms).
Endoparasites can exist in one of two forms: intercellular parasites (inhabiting spaces in the host’s body) or intracellular parasites (inhabiting cells in the host’s body). Intracellular parasites, such as protozoa, bacteria or viruses, tend to rely on a third organism, which is generally known as the carrier or vector. The vector does the job of transmitting them to the host.
Epiparasite:
An epiparasite is one that feeds on another parasite. This relationship is also sometimes referred to as hyperparasitism, exemplified by a protozoan (the hyperparasite) living in the digestive tract of a flea living on a dog.
Social parasites:
Social parasites take advantage of interactions between members of social organisms such as ants or termites.In kleptoparasitism, parasites appropriate food gathered by the host. An example is the brood parasitism practiced by cuckoos and cowbirds, which do not build nests of their own and leave their eggs in nests of other species. The host behaves as a "babysitter" as they raise the young as their own. If the host removes the cuckoo's eggs, some cuckoos will return and attack the nest to compel host birds to remain subject to this parasitism.
Adelpho-parasite
An adelpho-parasite is a parasite in which the host species is closely related to the parasite, often being a member of the same family or genus. An example of this is the citrus blackfly parasitoid, Encarsia perplexa, unmated females of which may lay haploid eggs in the fully developed larvae of their own species. These result in the production of male offspring. The marine worm Bonellia viridis has a similar reproductive strategy, although the larvae are planktonic.
Host Defenses:
Skin:
The first line of defense against invading parasite is the skin. Skin is made up layers of dead cells and acts as a physical barrier to invading organisms. These dead cells contain the protein keratin, which makes skin tough and waterproof. Most microorganism needs a moist environment to survive. By keeping the skin dry, it prevents invading organisms from colonizing. Furthermore, human skin also secretes sebum, which is toxic to most microorganisms.
Mouth:
The mouth contains saliva, which prevents foreign organism from getting into the body orally. Furthermore, the mouth also contains lysozyme, an enzyme found in tears and the saliva. This enzyme breaks down cell walls of invading microorganisms.
Stomach:
Should the organism pass the mouth, the stomach is the next line of defense. The stomach contains hydrochloric acid and gastric acids, which makes its ph level around 2. In this environment, the acidity of the stomach helps kill most microorganisms that try to invade the body through the gastric intestinal tract
Eyes:
Parasites can also invade the body through the eyes. The lashes on the eyelid prevents invading microorganisms from entering the eye in the first place. Even if the microorganism do get into the eye, tears contain the enzyme lysozyme, which will kill most invading microorganisms.
Immune system:
Should the parasite enter the body, the immune system is a vertebrate’s major defense against parasitic invasion. The immune system is made up of different families of molecules. These include serum proteins and pattern recognition receptors (PRRs). PRRs are intracellular and cellular receptors that activate dendritic cells, which in turn activate the adaptive immune system’s lymphocytes. Lymphocytes such as the T cells and antibody producing B cells with variable receptors that recognize parasites.
Adaption:
Parasites infect hosts that exist within their same geographical area (sympatric) more effectively. This phenomenon supports the "Red Queen hypothesis—which states that interactions between species (such as host and parasites) lead to constant natural selection for adaptation and counter adaptation." The parasites track the locally common host phenotypes, therefore the parasites are less infective to allopatric (from different geographical region) hosts.
Transmision:
Parasites have a variety of methods to infect hosts. For example, the Acanthamoeba enters the body when the environment is not hostile, and the strongyloides stercoralis enters the body when a host steps on infected ground while barefoot. Many parasites enter the food of their hosts and wait to be eaten. Plasmodium malariae uses a mosquito host to transmit malaria and Loa Loa parasites use deer flies to enter hosts.
Parasites inhabit living organisms and therefore face problems that free-living organisms do not. Hosts, the only habitats in which parasites can survive, actively try to avoid, repel, and destroy parasites. Parasites employ numerous strategies for getting from one host to another, a process sometimes referred to as parasite transmission or colonization.
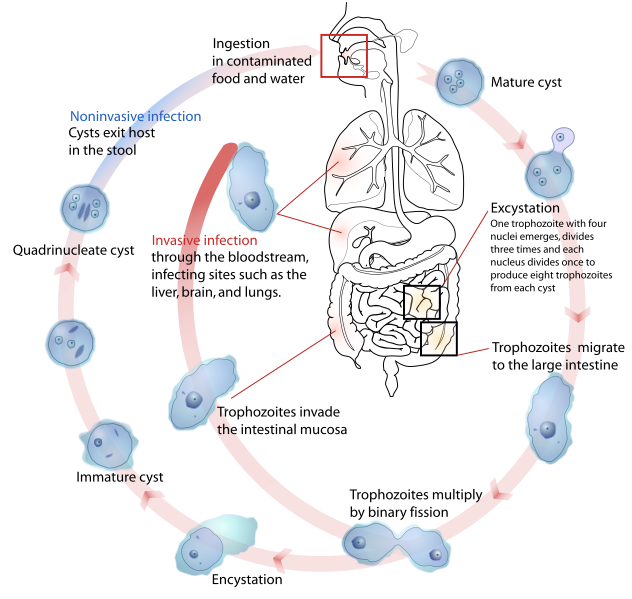
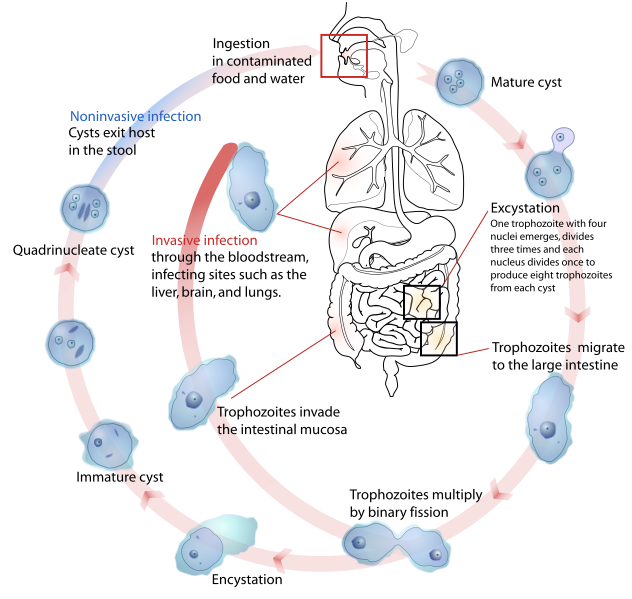
Some endoparasites infect their host by penetrating its external surface, while others must be ingested. Once inside the host, adult endoparasites need to shed offspring into the external environment to infect other hosts. Many adult endoparasites reside in the host’s gastrointestinal tract, where offspring can be shed along with host excreta. Adult stages of tapeworms, thorny-headed worms and most flukes use this method.
Among protozoan endoparasites, such as the malarial parasites and trypanosomes, infective stages in the host’s blood are transported to new hosts by biting-insects, or vectors.
Larval stages of endoparasites often infect sites in the host other than the blood or gastrointestinal tract. In many such cases, larval endoparasites require their host to be consumed by the next host in the parasite’s life cycle in order to survive and reproduce. Alternatively, larval endoparasites may shed free-living transmission stages that migrate through the host’s tissue into the external environment, where they actively search for or await ingestion by other hosts. The foregoing strategies are used, variously, by larval stages of tapeworms, thorny-headed worms, flukes and parasitic roundworms.
Some ectoparasites, such as monogenean worms, rely on direct contact between hosts. Ectoparasitic arthropods may rely on host-host contact (e.g. many lice), shed eggs that survive off the host (e.g. fleas), or wait in the external environment for an encounter with a host (e.g. ticks). Some aquatic leeches locate hosts by sensing movement and only attach when certain temperature and chemical cues are present.
Some parasites modify host behavior to make transmission to other hosts more likely.









_parasitized_by_Acrodactyla_quadrisculpta_larva_(RMNH.INS.593867)_-_BDJ.1.e992.jpg)